Well… better late than never, some say…! Here at UpDoc Media, we like to lay out some predictions to the year and typically these fall in the first week or so of each calendar year. Well… if your 2020 has been anything like ours…. January FLEW BY. So, with that and with gratitude for your patience and understanding of this particular post’s delay…
HERE ARE…. “20 Predictions for 2020.“
1. Adapt or Else
If you don’t adapt, you will be phased out. It’s not going to be catastrophically fast, as much as it’d be a frog in a pot of water slowly coming to a boil. “Adapt or Else” applies to all areas of practice:
- Clinical practice patterns
- Patient engagement
- Marketing and advertising
- Human resources and recruiting
- Finance and accounting
- Documentation and billing
- Local and regional public relations
- Practice/company branding
- Revenue activities
- Ecosystem of service options
- Patient/client market mix
The list goes on.
Ultimately, 2020 as both New Year and New Decade is some what of an arbitrary new start for provider organizations, patient consumers, payer institutions, and stakeholders at large. Everyone knows that healthcare is broken. So then… organizations that begin intentionally trending towards a new excellence in “wellcare”… such companies will being capturing the attention of payers and patients alike.
2. Accountability (PDPM, PDGM, Outcomes, Population Health)
We’ve been warned for years…. it’s coming. Well, it’s here. Whether it’s PDGM, PDPM, MIPS, upstream models of care, population health management, employee wellness… or, any other label… all this has to do with accountability with the mechanics dilemma.
After all, in healthcare, practices primarily keep the doors open by making money via the service of seeing patients. While many iterations have payment reform have tried to guide the industry towards keeping people healthy versus paying practices for billed visits… it has finally come to pass that regulation and revenue are now truly tied. In this, we’ve seen the unfortunate some less than prepared entities take drastic measure to keep up with the changes.
This is all to say, pretty much everyone has told us so. Now, we have to live up to it. NOW, we need to prove by the numbers we are worth every penny. For some entities, this will be a struggle. For others, life goes on as they’ve always lived. And yet, for others… this is a welcome challenge to emerge as an industry leader. Which one will you be?
3. It’s not as bad as you think it is.
Even with all these changes, it really isn’t as bad as one would think. This isn’t the first, second, nor even third big wave of change that modern healthcare has seen. It was only between 1965 and 2010 when Medicare and Medicaid became a reality and that the Affordable Care Act was signed into law. In fact, it was 30 years ago in the 1990s when the HMO storm front became a thing. And, for all that… we’re not even talking about the technological ways that healthcare has changed with improvements in immunology, anesthesia, wearables, oncology, general surgery, primary care, pediatrics, radiology, cardiology, and patient-provider communications.
Speaking of technology, A.I. and telemedicine/telehealth are very much in the spotlight for positive movement in the 2020s (more on this later).
We will adapt (or else)… and, we will help each other thrive. After all… society depends on us doing so!
4. Education will be changing it’s ways.
To say that student debt is out of control is perhaps the understatement of the decade. How out of control?? How about $1.6 TRILLION dollars out of control. #Yikes
The pricing and delivery for institutions of learning and research have become unsustainable. Those that have recognized this are changing their patterns of best practice; integrating virtual learning, distance learning, asynchronous classroom functions, etc. — and, are exploring novel methods of organization and administration of classroom cohorts. Of course, all of this is a problem of both regulation and accreditation… along with a myriad of other factors that continues to make higher education pricey (See: “Why Does Grad School Cost So Much?”) while seemingly inflating the value of such degrees.
5. Policy and Politics: A Personal Matter
For the first time in a long time, healthcare policy, politics, and legislative advocacy will matter at a personal level for healthcare professionals en masse. Just for fun, I asked a couple Facebook groups where they were — if they needed to take more ownership, if employers needed to play a bigger role, if the associations needed to up their game, or… if nothing would ever change and its perhaps too far gone. Here were the results:

So, where are you? Over 50% of your colleagues feel the need to become more involved… what are your next steps?
6. Advocacy is awareness. Awareness is advocacy.
It’s not longer a game of a small groups, tasked with big missions. Advocacy initiatives will fail if they do not have meaningful awareness inside our profession and externally to all our stakeholders.
This is a game that must be played both internally and externally.
The sad fact is that, culturally, our profession has never been taught to care enough about advocacy issues until it is either too late, or, directly affects our practice setting. Too often, if we are in outpatient and something happens in the world of acute care — it’s not our problem per se. The same goes for if something happens in outpatient and we hail from home health…. not our problem.
THIS EXACT MINDSET… IS. OUR. PROBLEM!
This is compounded by the fact that most of our colleagues aren’t aware or have tuned out advocacy issues. Therefore, this lack of functional awareness has severely limited our ability to initiate grassroots and profession wide action to legislators as well as to decision and policy makers. Certainly, keeping up with events can be tedious. However, we know where this road leads. We’ve been down this road. Arguably… this is the only road we know.
We know what happens if we don’t act, aren’t aware, or stop caring — I’d like to see what happens when we are aware, take action, and behold this as a personally core matter.
7. Own It or Lose It
If you don’t own it, someone else will take it from you. In many business frameworks and theoretical models, there are direct competitors and substitutions that companies should be aware of. These forces that may detract or disrupt your company many come from industry incumbents, new entrants, or even from outside the industry — something that is common with substitute products and services. Healthcare has come to a boiling point where multiple disciplines have competing interest on both a scope of practice standpoint as well as a revenue/operational standpoint. As such, professions that take true ownership of their abilities will have it properly reflect in their licensure — all of which is something that matriculate from policy, politics, and advocacy.
8. Talent will make their own choices.
The cat is out of the bag… and, has been for some time. With what many who have been incumbent in rehab therapy consider to be more or less job market mayhem… the emerging talent and developing professional have had enough; now doing due diligence in examining best fit for employers at a level never before seen. After all, UpDoc isn’t the only resource for job market / salary norms, talent survey reports, or insights practice management perspectives.
There plenty of brands exploring this space to give the many entities within our profession a veritable voice. The thing of it is, there seems to be quite the consensus — good talent is hard to find, and, good talent is hard to keep (more on this below). The biggest thing is now talent is now making their own employment portfolios. This isn’t exactly new per se. However, many employers have found that the effect has been far more pronounced in recent quarters — just as the “lifetime employee” evolved into the “career phase employee,” we are now seeing the “career phase employee” shift towards a “flexible lifestyle employee.”
9. Patients are and have always been smarter. Brands that disrespect consumer intelligence will suffer.
Again, this is nothing new. However, the way practices and organizations regard their customers / clients / patients / and prospective consumers will most certainly be changing this year. It wasn’t that long ago that patients felt as if they were a victim of their healthcare circumstance; terrified to leave examination rooms as if they would be breaking some type of rule, taking little initiative to guide or command a conversation with a healthcare provider, or, having only a slight idea of what their benefits truly entailed.
This has drastically changed in the last handful of years and is coming to a head with patients being very much savvy consumers of healthcare. Organizations that disrespect and/or even insult the intelligence of their customers… they will be in a world of hurt. I can still recall ages ago during my clinical affiliations when a patient left the clinic after seeing a physical therapist (not my C.I.) and exclaimed to on exit to the aide/tech as well as to the front desk:
“I’m SO GLAD I just paid $20 for a hot pad and traction… I could’ve done that at home.”
— Angry Patient, Sarcastically Spoken.
Value proposition is going to be huge in 2020. Under promising and over delivering will be the name of the game for patient care experiences.
PS. If you’re not convinced about how smart our patients are? Watch: THIS (starting at 1:30) via Dr. Vince Gutierrez.
10. EMR Battlegrounds
EMR companies have been at it for some time, and, it only takes a moments glance in any convention exhibit hall to notice that in the world of healthcare and rehab therapy — EMRs are not exactly as friendly to each other as they used to be. Some may even quip that they never were. Regardless of the feelings in this arena, we can simply expect that the competition in the world of EMRs is going to reach a new level.
Users are better features, an elevated user experience, quicker interface, customization, and have many more suggestions on top of all that.
If you want to make your voice be heard, consider contributing to our EMR Wish List Survey 2020!
11. The Fight For Talent
For 2020, recruitment is going to be insane. As mentioned in sections above, good talent is hard to come by. Organizations that make meaningful investments into their human resources will become big winners in the years to come. What do we mean by meaningful investments? We’re talking the clear pathways of growing into and upwards within a company. We’ll have future articles on this — but for now, just keep an eye on talent… a very watchful, genuine, caring eye….. authenticity is key here.
12. Residency Wars
When there are companies paying $74 for an FTE resident and others are paying $45k-55k/year… it gets difficult for a prospective resident to commit to not just that lowered pay, but to the 2 or 3 years of tenure to follow after residency as they either go down the track of simply working in that company or pursuing further training in fellowship. Most agree it’s good for the profession and for our patients. Most also agree that it isn’t exactly financially feasible for the long term. It can be expected that 2020 will demonstrate some truly interesting dynamics in the world of post-graduate training, specialization, education, and credentialing.
13. Collaborators win out big.
This has been mentioned many times in the past — in my old classic blog as well as in 2017’s PPS Recap. No singular entity has the answers for “all of it.” Our organizations as providers of healthcare and the infrastructure to provide health services stand to gain more by working together rather than by tearing each other apart. Of course, there’s human nature and the forces of competition in play. Nevertheless, companies that may have shared interests and classically considered competitors will very likely be seen to work together for the greater good — should their leadership see the historically repeated wisdom of such arrangements. Some, of course, will have incompatibility between them — others, will find ways to work things out. Much as we’ve seen so much consolidation in mergers and acquisitions, you can see a strong emergent wave become present in 2020 for collaborators wish big visions in winning big; not just for themselves, but for the people they serve.
14. The age of healthcare transparency.
The big news broke Fall of 2019 — Hospitals Must Post Their Real Prices Starting in 2021. Transparency has been a growing part of both consumers and companies alike — all doing their best to find ways to become more socially responsible. Transparency, however, doesn’t mean you open up the books. It means stop hiding stuff. It means owning up to the mistakes, past and present. It means admitting wrong and apologizing for whatever skeletons came out of the closet, usually years after one has taken up a management position.
Transparency also means coming up with collaborative solutions that include those that decisions would otherwise affect the most — healthcare’s line staff and patient consumers. If we’ve learned anything about corporate social responsibility, it’s this: People care about it and assuredly will vote with their dollars with increasing waves.
15. Decline of short term winners in the industry.
We’ve heard it before and we’ll hear it again: Don’t sacrifice long term success for short term gains. The long game involves years and years of difficult play calling and even more grit. Sometimes, this is too much for organizations and for key individuals to bear. Other times, there was never any intention to consider the long term. What we can most certainly expect is that the quick movers with sights set on short term gains will be declining in 2020 — healthcare just isn’t about that anymore. It’s not sustainable; and thus, anything that doesn’t interweave a sense of longevity and trustworthiness into its organizational standards shall begin its decline this year.
16. Outpatient will be blowing it up.
We’ve already observed a shift away from what individual clinicians have traditionally considered lucrative settings such as HH and SNF (more on this later). One can expect a strange sense of growth despite pulsatile job market saturation in the outpatient setting. Why? Costs. Not to the patient per se… to the payers who are providing coverage for their care.
Yes, we are predicting that outpatient services will be making some interesting gains this year… not in its traditional format, but in emerging roles such as in home care dispatch under outpatient billing; through telehealth and membership driven services; in upstream models of care; in population health management; and, in anything that might provide both cost-savings and human capital preservation on an economic level to heath systems at large.
17. Acute care will step up its game because they are as interventionally upstream as it gets.
My roots are in acute care. It’s a setting and specialty I have very much love for and have always seen incredible potentials in helping health systems, hospitals, patient consumers, and payers save money AND make money.
10 years ago, literature showed that Physical Therapists with discharge planning responsibilities added a lot of value to the flow of patient care — becoming a cost-saving factor in discharge planning where cases not following a Physical Therapist’s discharge recommendations were 2.9 times more likely to become re-admitted to the hospital within 30 days. More recent studies have suggested that one could expect… “significantly higher readmission rates… for patients whose interdisciplinary team did not have a physical therapist…”
This, combined with the rapid emergence of Physical Therapist’s practicing in the Emergency Department (to which I had the privilege of experiencing) — such involvements of PTs for clinical effectiveness at the system level, at the medical team level, and for the patient experience has been shown to be EXCELLENT and necessary… it’s not a nice to have anymore.
If you’re interested in #PTinED, consider connecting with Carleen Jogodka and Stacie Fruth.
18. HH/SNF continues to struggle.
No one wanted to believe it. The day finally came. Cash flows changed, people got laid off. And, the tragedy is that many may be quickly hired back, which will only cause MORE of a cash flow problem. 2020 is going to be a year of rough adjustment for home health agencies, home care staffing companies, and SNFs in general. There’s a lot of scrutiny coming from many angles and there seems to be quite the microscope on these rather related settings in rehab therapy. Scrutiny is never a welcome experience, neither is auditing. That said, both home health and skilled rehab are key links across the continuum of care. They won’t be going anywhere any time soon… but, this year will be a proving grounds of sorts.
19. Telehealth will finally emerge as a solid part of the industry’s practice pattern.
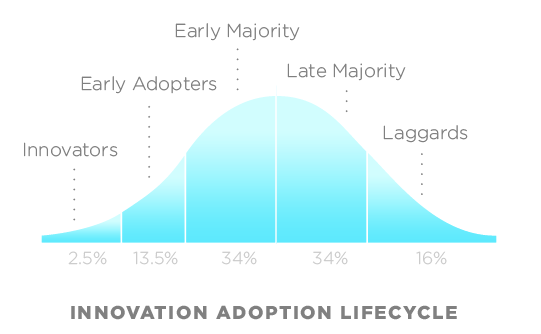
People (us included) have been telling everyone to watch out for telehealth, asynchronous visits, etc for a LONG time. This is the year and the decade that this topic will grow past the early adopters.
With many demographic brackets now heavily involved in use of mobile technology, wearables, and multiple channels of digital communications — the marketplace is ready for both patients and providers to engage digitally and virtually, both synchronously and asynchronously. This, of course, comes with many questions about compliance and privacy — yielding an arena with many shades of gray and few experts to rely upon in “doing things right.”
Still not convinced? How about this breaking news.

20. Upstream, subscription, and direct-to-employer models will have it’s wave of emergence.
Upstream models of care and wellness was strongly seen as an emerging opportunity during the 2019 Private Practice Section conference. This lines up with the accountability and transparency we’re seeing for this year (and, decade). This also lines up with what payers are looking to establish as a new standard within healthcare; and, it something that patient consumers very much want as well. As many like to make puns about, healthcare is too much about the sick and not enough about making people healthy. Our final prediction for 2020 is that practices, providers, and organizations will begin seeking out their capabilities to deliver in this emerging landscape — scary as it will be, it goes back to our prediction of collaborators by where shared risk and shared reward will yield much fruit.